Benefits Of Using Electronic Health Records (EHRs) Explained

 Every person has a record of their medical history, which provides doctors, nurses, and other healthcare staff background information about their physical and mental well-being.
Every person has a record of their medical history, which provides doctors, nurses, and other healthcare staff background information about their physical and mental well-being.
However, the traditional method of writing these details down on pieces of paper had many flaws, including not being able to be passed on to other medical staff and easily getting lost.
That is why, since Electronic Health Records (EHRs) started to become widespread, it has revolutionized the healthcare sector.
What is the history of EHRs?
The history of EHRs can be traced back several decades, with the development and adoption of EHR systems evolving gradually over time. Here is an overview of the key milestones in the history of EHRs:
1960s and 1970s: Emergence of Early Concepts
- The concept of electronic health records began to emerge in the 1960s and 1970s as healthcare professionals recognized the potential benefits of digitizing medical records.
- Early attempts at electronic records involved rudimentary computer systems that stored patient data in a digital format, but these systems were not widely adopted due to limitations in technology and cost.
1980s: Early EHR Systems
- In the 1980s, more sophisticated EHR systems started to appear. However, these systems were often institution-specific and lacked interoperability with other healthcare organizations.
- Prominent EHR systems during this era included the Regenstrief Medical Record System and the HELP (Health Evaluation through Logical Processing) system.
1990s: Advancements and Standardization
- The 1990s saw significant advancements in EHR technology, with greater emphasis on standardization and interoperability.
- The Health Level 7 (HL7) standard emerged as a key protocol for healthcare data exchange, facilitating interoperability between different EHR systems.
- The Institute of Medicine (now the National Academy of Medicine) released a report in 1991, “The Computer-Based Patient Record,” which promoted the adoption of electronic records and set the stage for future developments.
2000s: Federal Initiatives
- The early 2000s marked a turning point for EHR adoption in the United States. The federal government launched initiatives to promote EHR adoption, including the establishment of the Office of the National Coordinator for Health Information Technology (ONC) in 2004.
- In 2009, the Health Information Technology for Economic and Clinical Health (HITECH) Act was enacted as part of the American Recovery and Reinvestment Act (ARRA). HITECH provided financial incentives to healthcare providers who adopted and demonstrated meaningful use of certified EHR technology.
- Major EHR vendors like Epic Systems, Cerner (Now Oracle), and Allscripts gained prominence during this period, and EHR adoption in healthcare facilities began to increase significantly.
2010s: Widespread Adoption and Standardization
- The 2010s witnessed widespread adoption of EHRs in healthcare settings across the world. The transition from paper to electronic records became a global trend.
- Standardization efforts, such as the introduction of the International Classification of Diseases, 10th Revision (ICD-10), and the adoption of SNOMED CT (Systematized Nomenclature of Medicine Clinical Terms), further improved data interoperability.
- EHRs evolved to encompass a wide range of features, including clinical decision support, electronic prescribing, and patient portals, enhancing patient engagement and care quality.
2020s: Continued Evolution
- In the current decade, EHR systems continue to evolve, with a growing focus on interoperability, data exchange, and patient-centric care.
- The COVID-19 pandemic accelerated the adoption of telehealth and highlighted the importance of digital health records for remote patient monitoring and care coordination.
- As of 2021, 96% of all non-federal acute care hospitals and nearly 4 in 5 office-based physicians in the US have implemented a certified EHR system.
Today, EHRs are a fundamental component of modern healthcare, contributing to improved patient care, data-driven decision-making, and the overall efficiency of healthcare delivery. As technology continues to advance, EHRs are expected to play an increasingly central role in the healthcare landscape, facilitating innovations such as artificial intelligence and predictive analytics in healthcare.
 What are the benefits of EHRs?
What are the benefits of EHRs?
In today’s rapidly evolving healthcare landscape, the adoption of EHRs has become increasingly essential for healthcare providers. EHRs offer a multitude of benefits that not only enhance patient care but also streamline administrative processes, ultimately leading to improved healthcare outcomes.
Enhanced Patient Care – The foremost benefit of EHRs is their ability to elevate patient care to new heights. By digitizing and centralizing medical records, EHRs grant healthcare providers quick and seamless access to a patient’s complete medical history. This accessibility empowers physicians to make more informed decisions, reduce the risk of errors, and ultimately enhance the overall quality of care. The availability of past diagnoses, treatment plans, and medication history ensures that patients receive tailored, effective treatments.
Streamlined Workflow – EHRs streamline the often complex and time-consuming administrative tasks within healthcare facilities. No more rifling through stacks of paper records or deciphering illegible handwriting. EHRs allow for automated appointment scheduling, efficient billing, and simplified insurance claims processing. This not only reduces paperwork but also minimizes the potential for errors, improving the efficiency of healthcare operations.
Accessibility Anytime, Anywhere – One of the most significant advantages of EHRs is their accessibility. Healthcare providers can access patient records securely from anywhere with an internet connection. This mobility is invaluable for doctors and nurses on the move, ensuring they have critical patient information at their fingertips, even in emergency situations.
Improved Accuracy and Legibility – Handwritten paper records can be challenging to read and are susceptible to errors. EHRs eliminate these issues by ensuring that all entries are legible and standardized. The enhanced accuracy reduces the likelihood of medication errors, misdiagnoses, and other mistakes that can have serious consequences for patients.
Efficient Data Management – EHRs offer robust data management capabilities. Healthcare providers can track and analyze patient data over time, identifying trends and patterns that inform treatment decisions. This data-driven approach to healthcare leads to more personalized treatment plans and improved patient outcomes.
Enhanced Communication and Collaboration – EHRs facilitate better communication among healthcare providers. They allow for the secure sharing of patient information, test results, and treatment plans, ensuring that everyone involved in a patient’s care is on the same page. This seamless communication reduces the likelihood of miscommunication and improves the continuity of care.
Cost Savings – While the initial implementation of EHR systems can be costly, they often result in significant long-term cost savings. Reduced paperwork, improved efficiency, and fewer errors can lead to lower operational costs for healthcare facilities. Additionally, EHRs can help prevent duplicate tests and unnecessary procedures, reducing overall healthcare expenses for patients and providers alike.
Enhanced Security and Privacy – EHRs are designed with robust security measures to protect patient data. Access is typically controlled through user authentication and authorization protocols, and data encryption ensures patient information remains confidential. This heightened security helps healthcare facilities comply with privacy regulations and build trust with patients.
Enhancing EHRs for Optimal Benefit Realization
 Having explored the multitude of benefits that EHRs bring to the healthcare sector, it becomes evident that there is room for improvement in this technology to maximize its usability and increase its adoption.
Having explored the multitude of benefits that EHRs bring to the healthcare sector, it becomes evident that there is room for improvement in this technology to maximize its usability and increase its adoption.
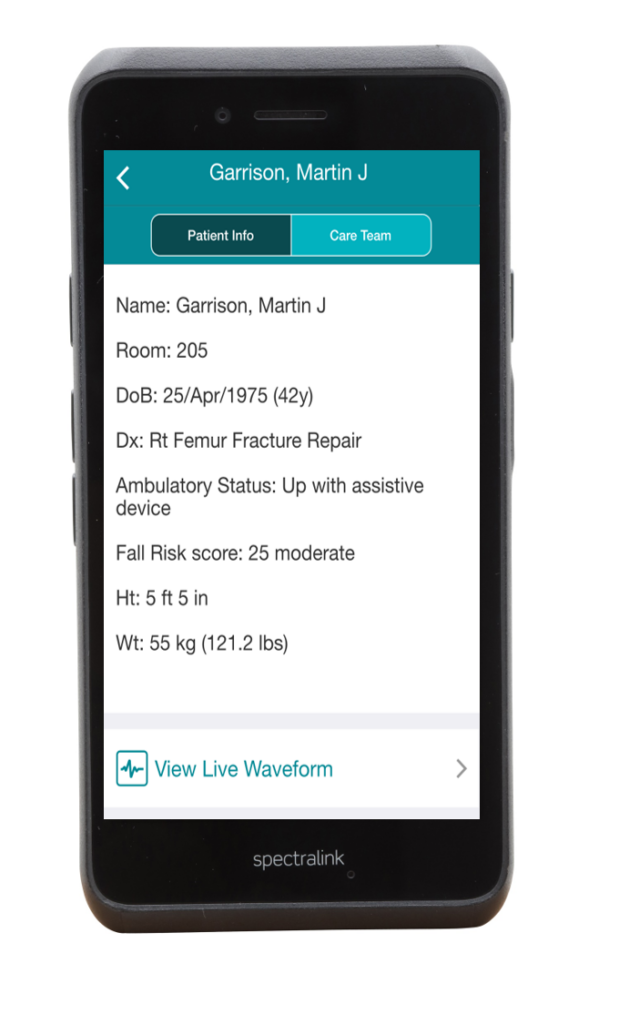
Originally designed for desktop computers, EHR systems have evolved to cater to the mobile era. A pivotal advancement lies in optimizing EHRs for smartphones, offering clinicians the advantage of having crucial patient information at their fingertips. This accessibility is especially valuable when they are visiting wards, making home calls, or collaborating with fellow professionals.
The significance of mobile EHRs cannot be overstated. Physicians and medical staff are often on their feet, requiring data access wherever they are rather than being tethered to an office. With EHRs on their smartphones, they can review patient vital signs en route to the patient, eliminating the need to locate a desktop computer.
Moreover, these handheld devices must be equipped to withstand the typical healthcare environment. Key features include screens compatible with gloved hands, extended battery life, and the ability to track lost smartphones to safeguard patient data.
Clear voice quality is essential for effective communication with pharmacies, patients, and other healthcare professionals. Additionally, the capability to scan information, such as patient bracelet barcodes, and instantly transfer it to the device further enhances efficiency.
In the dynamic healthcare setting, durability is paramount. These smartphones must endure accidental drops and rough handling. Waterproofing is another essential feature, ensuring functionality even if they find themselves submerged in a sink or toilet.
Ultimately, reliability is the linchpin. Clinicians rely on these devices to access EHRs throughout the day, enabling them to retrieve vital signs, images, and medical history promptly for each patient encounter.
This enhancement in EHR accessibility empowers healthcare professionals to leverage the full spectrum of benefits. It accelerates patient care, ensures the delivery of the most appropriate treatment, and helps identify critical red flags that might otherwise go unnoticed.
In conclusion, refining EHRs to align with the demands and challenges of the modern healthcare landscape is essential. By making EHRs more accessible, durable, and reliable, we can further harness their potential to enhance patient care and improve healthcare outcomes.
